-
outcomes
10/10/2014 at 03:02 • 0 commentsWhat if you could, statistically at least, eliminate type one?
more to come.
-
evolution
10/10/2014 at 02:59 • 0 commentsfrom a fly box to...
more to come.
-
FDA
10/10/2014 at 02:56 • 0 commentsreal progress... the start of a new age of healthcare devices and technology?
more to come.
-
pebble
10/10/2014 at 02:55 • 0 commentsmore to come, lots of fun at pebble dev retreat 2014!
-
Prospect
09/23/2014 at 15:41 • 0 commentsA summary of where we are, and where we're headed.
As I plan out my final video for the semi-final portion of the hackaday prize, I find it difficult to focus on one particular aspect of the build for very long, as there are many exciting aspects, and my mind simply races with the possibilities, the prospects of this project.
We made our rig smaller:
![]()
And with a sweet case design, we can make it better still.
![]()
We've also found many new ways to present the data....
Evan was running low after a busy night, I was drowsy and not paying attention to the iPad on our entertainment center, nor was I cognizant of the buzzing pebble on my wrist... but this got my attention:
Once the CGM data has been liberated, the sky is the limit. We can use off the shelf "internet of things" devices, or augment everyday items ourselves.
We can tap into common device features, such as the new iOS "widgets," to offer yet another quick view of realtime data (we can do the same for Android!):
![]()
The online community that has taken these tools as their own and evolved them, is now nearing 7,000 people. A formidable group, with potential resources to rival some of the big players in this field. So... we begin chatting with the FDA and finding more ways to trial and research our wild ideas, while continuing to drive the conversation about where Open Source and regulated devices or systems converge.
We are at a unique and critical moment, where we can help evolve a process to promote, not stifle, the innovations most desperately needed by those with type 1 or other chronic conditions.
The true prospect is the great change possible across the medical & healthcare industry, where patient data has been liberated and innovators, particularly those on the front lines, have an unencumbered path to victory.
-
Packaging
09/21/2014 at 22:38 • 0 commentsType 1 diabetes is burdensome. When designing tools to help manage it... don't add to the burden, okay?
Seems simple enough, but most of the tools a diabetic is given are not designed with this in mind. They're intended to keep a person alive, which is certainly a good thing, but the actual usability is often lacking.
The truly awesome Scott Hanselman nails it:
http://www.hanselman.com/blog/TheSadStateOfDiabetesTechnologyIn2012.aspx
So, when building an ambulatory system, which by definition, is to be taken with the patient, it needs to benefit beyond the burden.
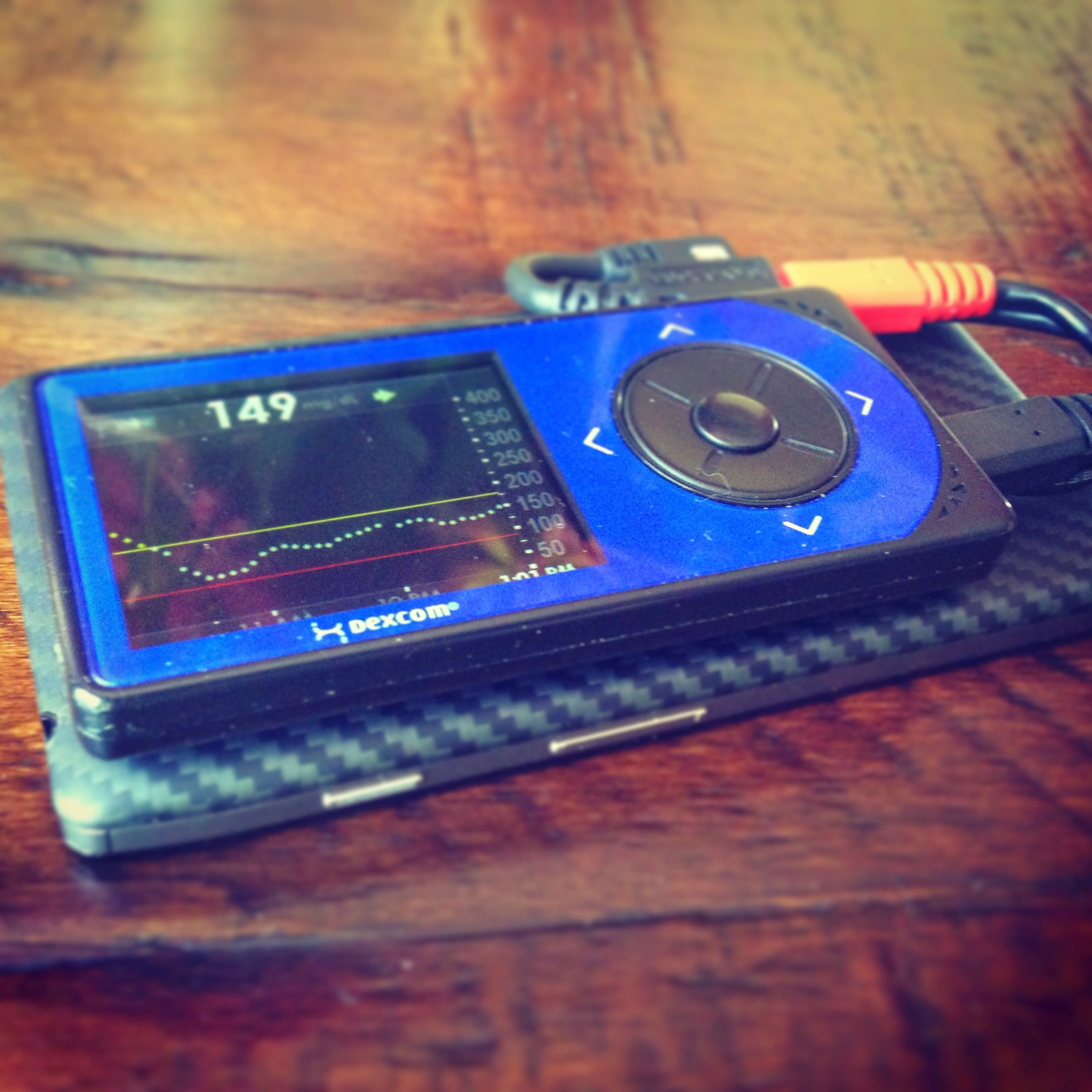
Our very first pass at combining the CGM and an Android phone:
We put this in a pouch, and it worked well... until we discovered the G4's biggest weakness: the USB port. Apparently, even normal force and use can snap these bad-boys off of the PCB. So, in this configuration, it took about 2 weeks to snap it off...
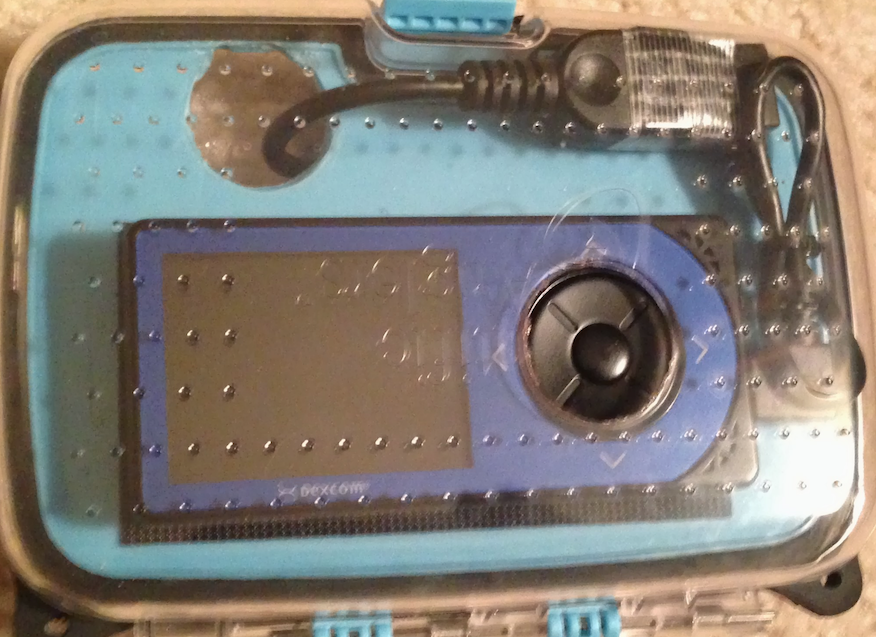
I went to amazon and searched for "small plastic cases" and after hitting a few variations on those terms, I found this:
![]()
It's a "Fly Box" and comes it several sizes, and living in the Finger Lakes region, the waterproof 'feature' would come in handy.
![]()
We ended up using two cases, one to maintain the waterproof-ness, and another for day to day use that allowed access to the control pad on the CGM:
![]()
And this worked well for kindergarten, when combined with a "fanny pack" that holds other essential supplies, it made it easy for Evan to keep with him. He rarely wears it, but it is a nice option to have.
![]()
For 1st grade, we wanted to shrink it down further - custom PCBs & 3D printed cases came to mind, but for our hack, these fly cases work well and don't cost very much (~$20).
The trick then is to find a SMALL Android phone with OTG capabilities. They're rare, and the trend in phone design is headed in the wrong direction... as far as this project is concerned. So, we dip back in time and try out an Xperia Ray (c. 2011). The G4 & Xperia Ray are very similar in size, so I put them in the smallest fly box (~3x5)... it works great, and is much smaller than "last years" model.
![]()
![]() Now, the Ray is a less than ideal selection for other reasons:
Now, the Ray is a less than ideal selection for other reasons: it must be "rooted" to work
The battery is small (~13 hours before needing recharge)
It's old
So, when I first began helping people get their own ambulatory system setup, I recommended the Moto-G.
Not too big, inexpensive off contract, and a quality product. It has proven so popular that others have come up with this:
![]() Beautiful! And a testament to the benefit of making all of this open & crowd sourced. Brilliant people contribute their skills to project and share it with thousands that may benefit.
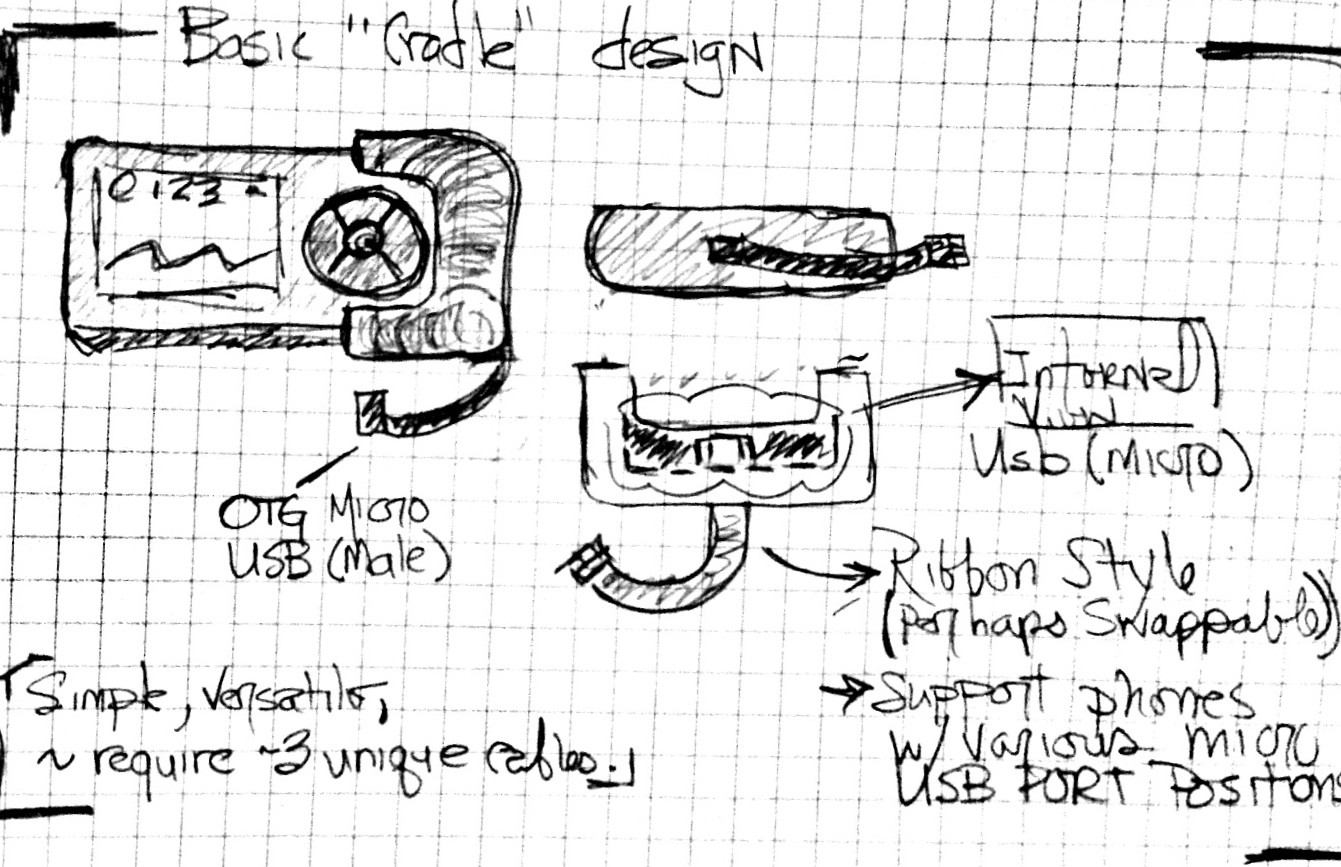
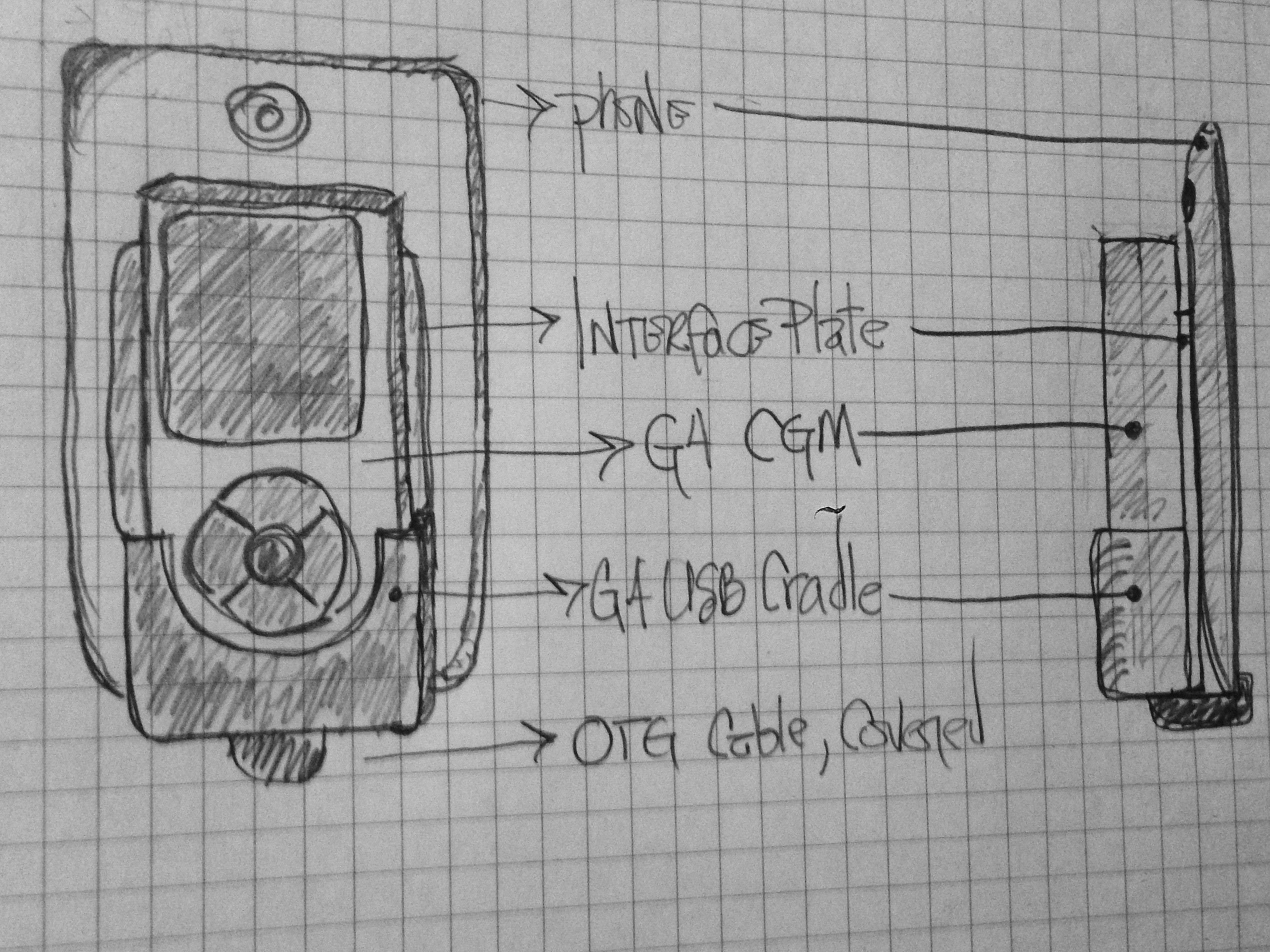
Beautiful! And a testament to the benefit of making all of this open & crowd sourced. Brilliant people contribute their skills to project and share it with thousands that may benefit.Here's a rough sketch of a universal cradle design. Primary purpose is to remove the wear and tear and undue force on the G4 receiver's USB port.
With a few cables to choose from, we can connect to most phones. I think bottom ports are most common on phones, but there are a few with side mounts (Xperias come to mind) that I'd like to handle, too.
![]()
-
UI Refinement
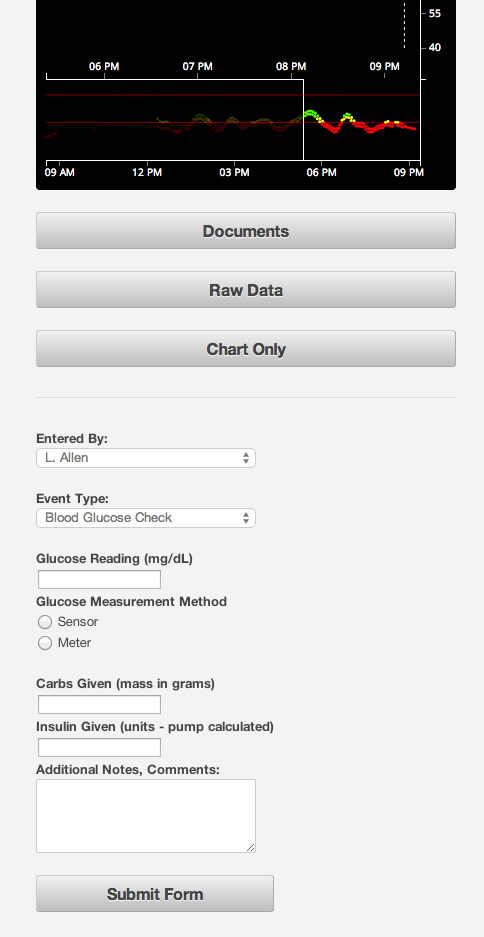
09/15/2014 at 03:09 • 0 commentsWe made significant updates to our system this past summer - a streamlined web app interface, a more portable and reliable "rig" were our highest priorities.
Here I'll discuss a few of the changes we made to our web views...
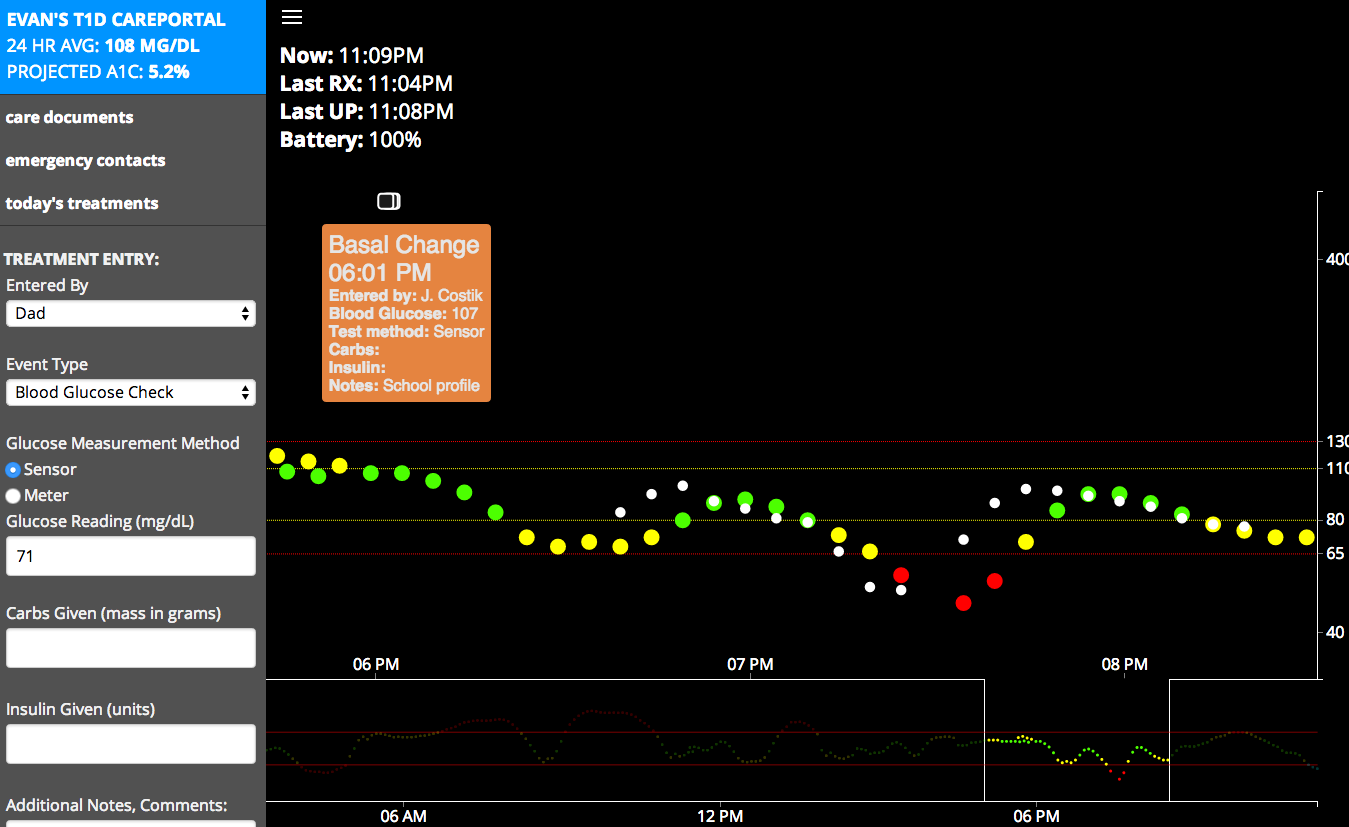
Current chart & care-portal:
![]()
Grabbing all the data is only useful if it is actionable. Making a useable chart view or watchface is not always as simple as it seems. What works for me, may not work for my wife, the school nurse or others.
Our initial view was simply blood glucose and trend,
We added a chart as others began to participate and collaborate (Lane D. Ross N. of Nightscout fame), and we added a "care-portal" to pull in even more diabetes data in real (or close to it!) time.
Our initial care-portal, used for Kindergarten:
![]()
The squares on the chart are treatments: insulin dose, food, blood glucose check, or even notes or questions. Once someone enters it, it is added to the chart, and a tooltip will be displayed when clicked or tapped. I made sure the site was responsive, as we like to log or view data from whatever device is handy.
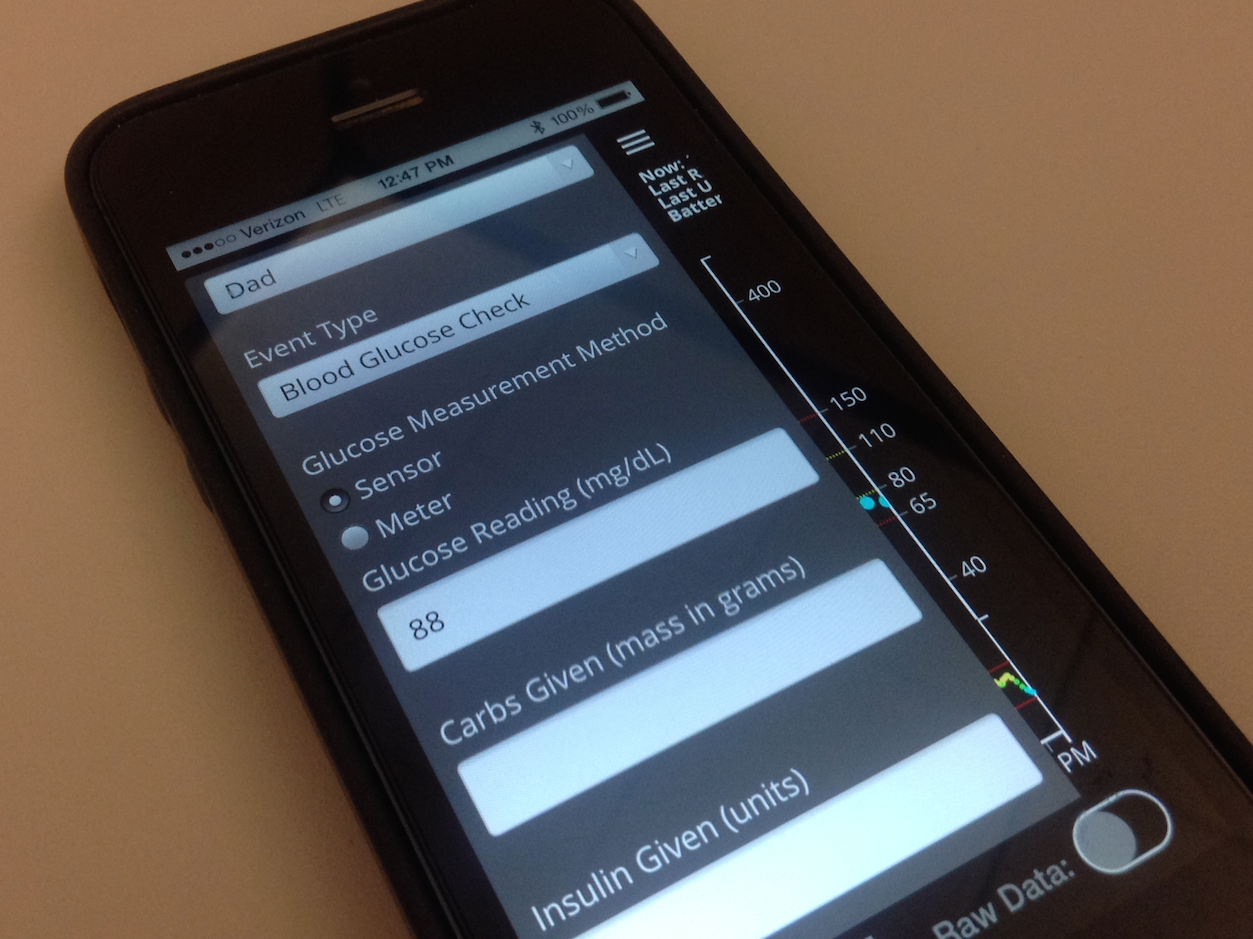
Recent updates followed this responsive design, while also allowing for a faster logging experience and use of CSS media queries allows us to customize for devices, even for orientation.
Here's a look at the menu on an vertically oriented smartphone:
![]()
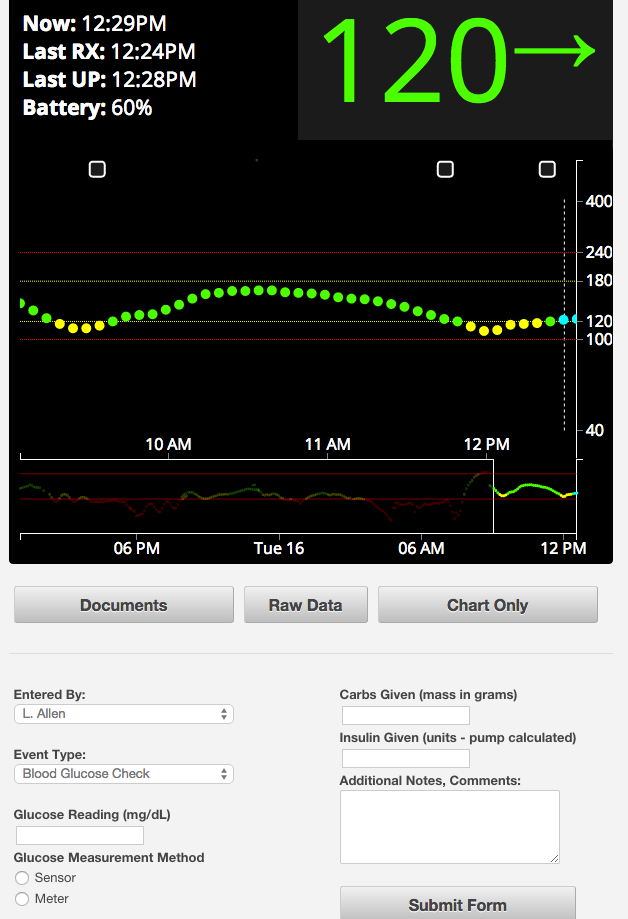
In landscape mode, we display a larger chart for better retrospective analysis and scrubbing:
![]()
A larger tablet screen gives us the best of both worlds - a large number and arrow for the current blood glucose data, and a big chart for a quick look or deeper dive into the data:
![]()
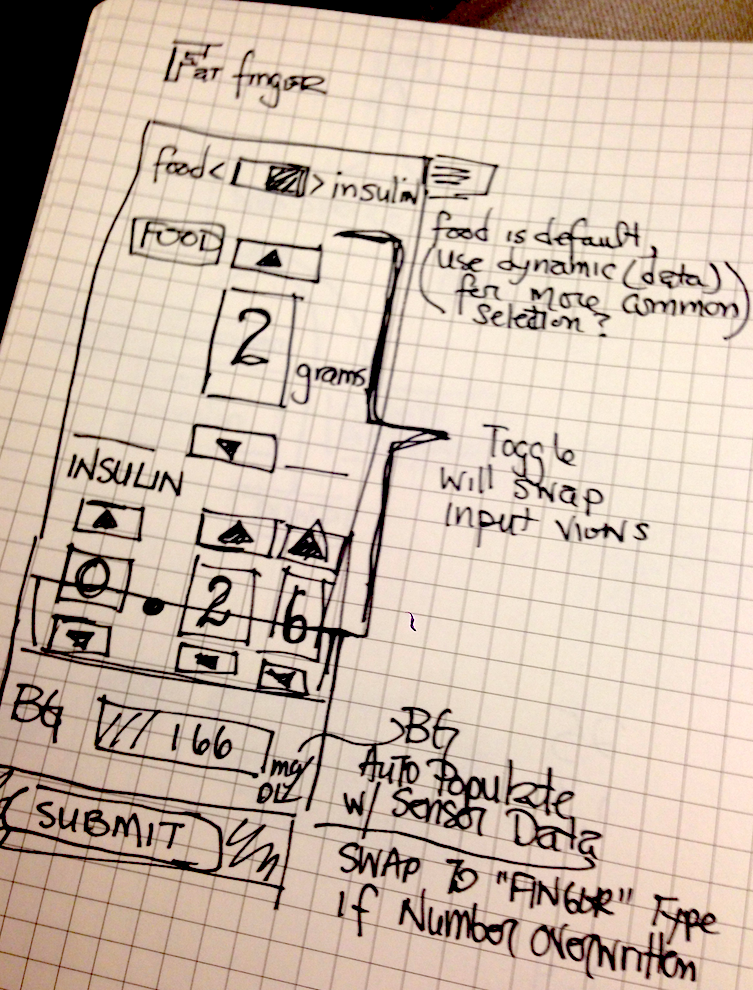
One enhancement currently in progress is a "time of day" customization of the menu, more specifically the treatment logging.
As person with diabetes or parent of a child with diabetes can tell you - overnight can be a challenge. Without a continuous glucose monitor, many of us set alarms to make finger check measurements to ensure blood glucose is in a safe range. Now, with a CGM, it alerts us to possible highs and lows, and, bleary eyed, we make corrections. We either give insulin for a high or glucose for a low - and logging this data accurately in a sleepy stupor can be tricky. What if one parent corrects right after the other, not knowing a correction was already made?
Laura suggested a "fat finger" interface, and I am current;y working to make that interface come and go by time of day:
![]()
-
An Unmet Need
09/08/2014 at 20:45 • 0 commentsTwo of the three primary pieces of our system have become widely used by people with diabetes, and more commonly, parents of children with diabetes.
What about this system strikes a chord with those impacted by type 1? Let me explain...
Type 1 diabetes robs a person's body of the ability to regulate blood sugar. Through no lifestyle or dietary "mistake," the body's immune system begins to attack the insulin producing cells of the pancreas.
No insulin? Sugar is stuck, it cannot pass to cells and be metabolized. Blood sugar, or blood glucose will continue to rise, an unquenchable thirst takes over to force sweat and urine to pour as much sugar out as possible. It is fruitless ultimately, and your body begins to consume muscle for energy, your blood becomes dangerously acidic, and it kills you.
Less than 100 years ago, if you had type 1 diabetes, it was going to kill you.
Fortunately, we now have insulin analogues and other wonderful technology to help us manage and survive with type 1 diabetes. I am thankful to all the scientists, engineers and motivated people that have made life with type 1 "better."
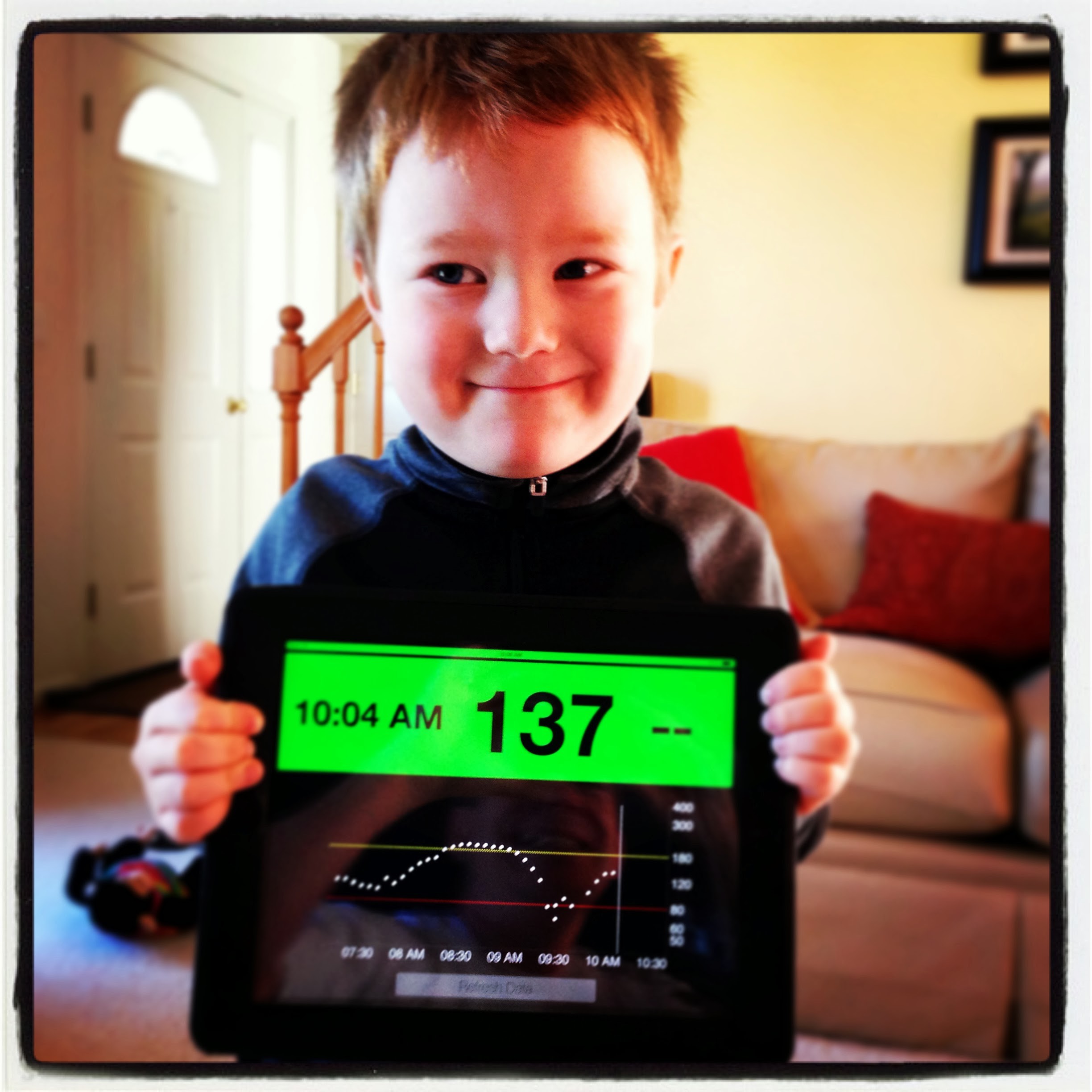
I am thankful, because I can continue to enjoy life with this amazing person, my son Evan.
![]()
When he was diagnosed, life changed.
My wife, Laura, and I immediately felt, saw the deficiencies in the processes, the standards by which type 1 diabetes is managed. So much data was generated and tossed away everyday.
We began to collect and log all of Evan's pertinent nutrition data. How much insulin does n carbs require... at this time of day? Was he active? What was the activity? Is he nervous, excited, happy, sad? Measurable or not, we tried to take note - and find the factors that weighed heaviest on Evan's blood glucose levels.
From a simple website to log data, to sophisticated web apps and deep analysis of the collected data... we saw that even modest use of these tools shifted outcomes so rapidly in Evan's favor.
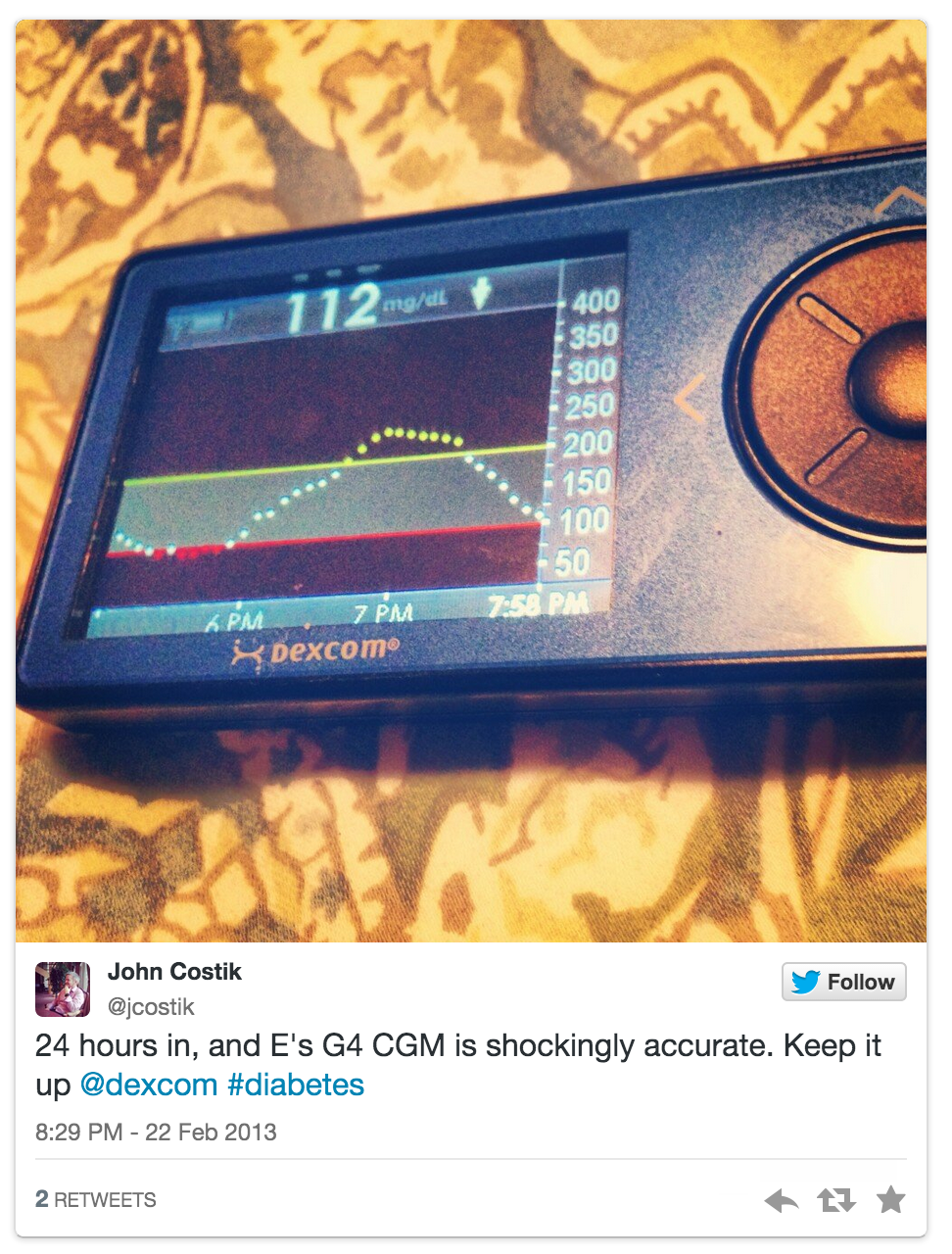
And then we discovered the G4:
![]()
A continuous glucose monitor, offers a frequent look at blood glucose levels - this feature alone makes it a worthy (should be standard!) weapon in the war with t1d.
By removing the location limit enforced by the standard receiver, the android + g4 receiver was just as life changing as the CGM alone.
What we grieved for in those early days after diagnosis... the limits t1d places on a child's life, the lives of all of us in the family... many of the limits evaporated. My wife and I can go out on dates, Evan can go on sleepovers, play on the hill with his sister... for hours, just as his mother and I did as kids. We thought those things were gone, but here they were again.
When word of these tools got out; after a few tweets over the course of 2013, hundreds, now thousands of families and individuals have found the power of these tools. Nurses at school, grandparents in Texas, a girlfriend in Australia... all these people can be connected to a person with diabetes single most important piece of data: their blood glucose. Helping to keep them safe, watching their back if so desired.
What if one day, the life you thought you knew, was taken from you? What if you found away to take it back? What happens when you make it open source and set it free for others like you? This happens:
https://www.facebook.com/groups/cgminthecloud/
![]()
-
Views
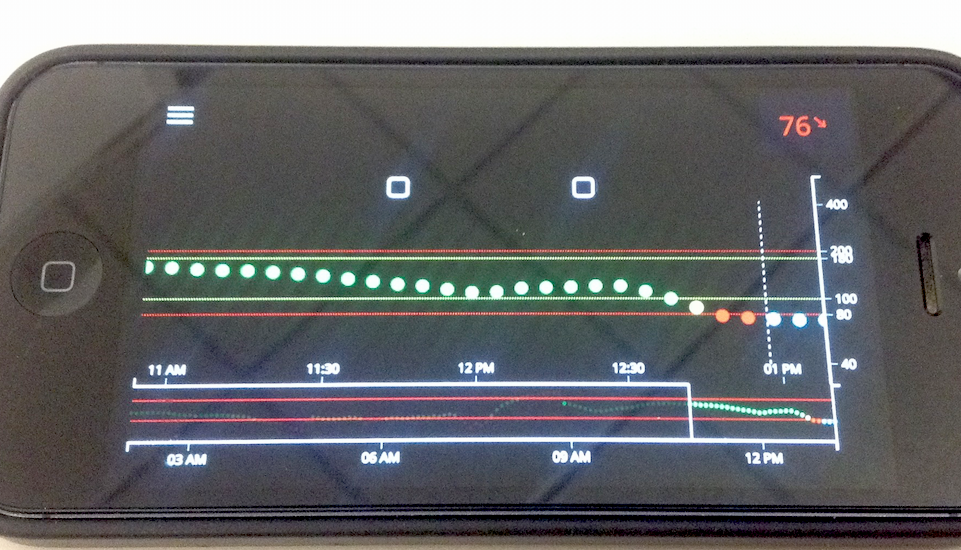
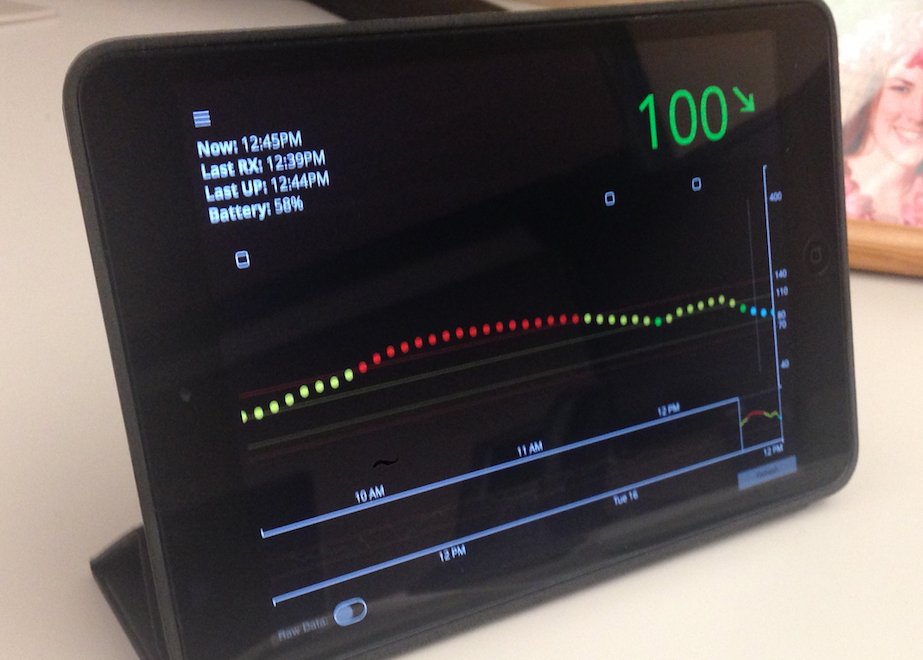
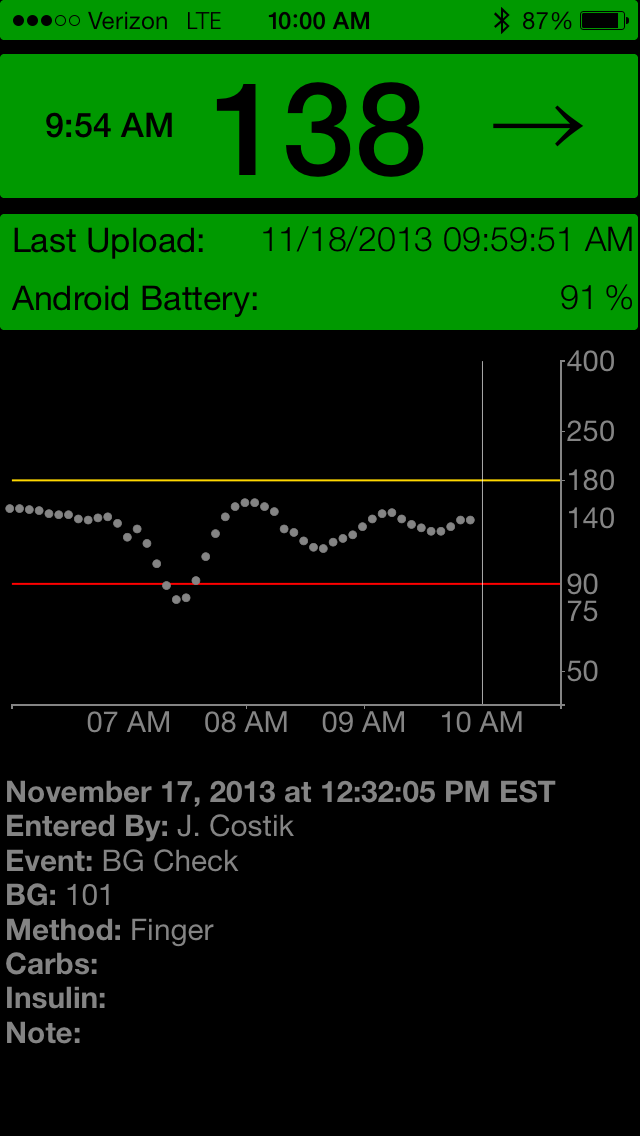
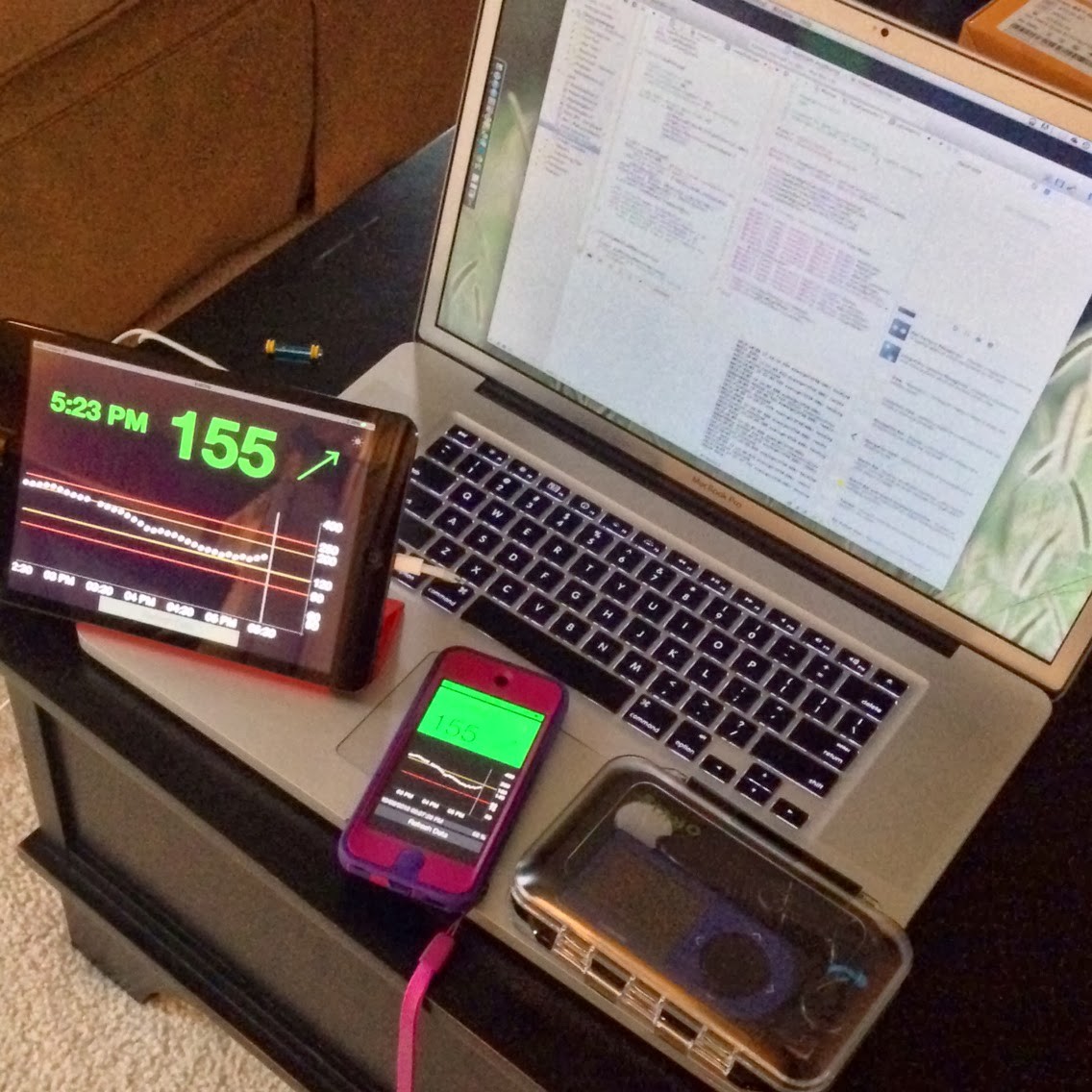
08/21/2014 at 01:20 • 0 commentsOnce the data was being published to the cloud, in our case, Azure - we set about creating glance-able views of the data.
Our iOS app makes wonderful use of push notifications to inform us of potentially dangerous blood glucose values, as well as system failures.
But the pebble watch made monitoring our son's blood glucose [BG] very passive, and took back much of the time we spent actively monitoring his BGs. Vibration alerts would notify us of events or conditions that required our attention.
![]()
![]()
![]()
-
Refining for Kindergarten, Collaboration
08/21/2014 at 01:14 • 0 commentsAfter tweeting about our success, we were contacted by Lane D. He was in search of code, like ours, that would allow him to remotely monitor his son.
We shared our code, and he shared a great set of chart view (using d3 - data driven documents) code that we were able to leverage.
We created a "care portal" for the school nurse (or ourselves) to log treatment data - insulin doses, nutrition, finger blood glucose checks, etc. Its responsive design making it very easy to use across device types.
![]()
![]()
Diabetes Data, Everywhere
A Continuous Glucose Monitor, the Cloud = Life Saving, Life Changing Diabetes Care... for everyone.
 John Costik
John Costik


 We put this in a pouch, and it worked well... until we discovered the G4's biggest weakness: the USB port. Apparently, even normal force and use can snap these bad-boys off of the PCB. So, in this configuration, it took about 2 weeks to snap it off...
We put this in a pouch, and it worked well... until we discovered the G4's biggest weakness: the USB port. Apparently, even normal force and use can snap these bad-boys off of the PCB. So, in this configuration, it took about 2 weeks to snap it off...



 Now, the Ray is a less than ideal selection for other reasons:
Now, the Ray is a less than ideal selection for other reasons:  Beautiful! And a testament to the benefit of making all of this open & crowd sourced. Brilliant people contribute their skills to project and share it with thousands that may benefit.
Beautiful! And a testament to the benefit of making all of this open & crowd sourced. Brilliant people contribute their skills to project and share it with thousands that may benefit.