The Problem:
Pneumonia has been the cause of death for over two
million children below the age of five.
Most of these
deaths occur in developing nations in South East Asia and
Africa.
Delay in diagnosis and lack of continuous
monitoring increase the risk and cost of treatment. Early
detection and providing timely treatments can reduce the
mortality rate of pneumonia .
Community healthcare
workers face a huge challenge in assessing and treating
children in low to medium income countries.
Existing Systems:
Primary method for diagnosing pneumonia is by
assessing whether the child has an elevated respiration rate
greater than or equal to 40 breaths/min. The NPB-290 Nellor pulse oximetry device is a low cost stationary pulse oximeter that is currently being used.
For respiration sensing chest based Impedance Pneumography method is used in conjuction with ECG monitoring systems. Nasal thermistor based systems along with Hot wire anemometers have been commercially been used to find respiration rate.
Background:
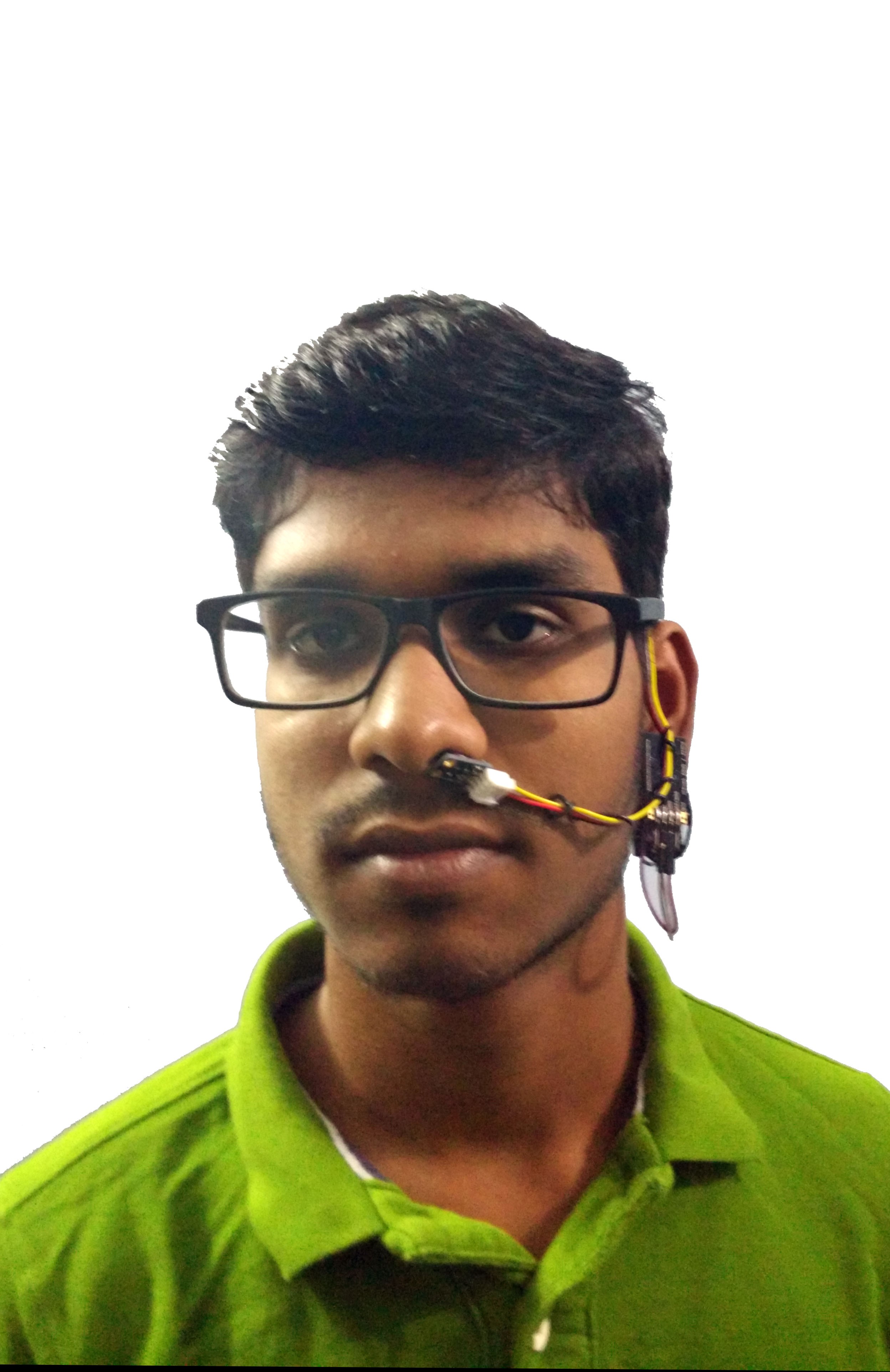
I, Vignesh am a final year engineering student from Chennai, India. I've always been into biomedical sensing and combining electronics and biomedical engineering.
Inspired after playing Deus Ex: Human Revolution as a 16 year old, My adolescent my mind was blown away by the possibilities in front of me. Reading about the work done by Dr.Hugh Herr at the Biomechatronics lab and Dr.Rosalind Packard at the Affective Computing lab MIT media lab. I realized I wanted to work on wearable sensors, After seeing the unbelievable progress in Machine Learning for the past few years empowering doctors with Machine Learning for diagnostics is my current goal.
Along the way I've read statistics on pneumonia and wanted to do my path, I've also been forming a team to aid us in this.
Solution:
There was a need for an inexpensive yet accurate wearable
diagnostic device which can continuously monitor vital parameters like Respiration Rate, Heart Rate, Blood
Oxygenation and Body temperature to accurately identify
pneumonia and thus enabling timely treatment.
Providing
timely aid can make the difference between life or death for
the child. Human and monetary resource which is limited in
LMIC can be conserved by facilitating remote
monitoring, thus enabling healthcare workers to provide
better care to the community.
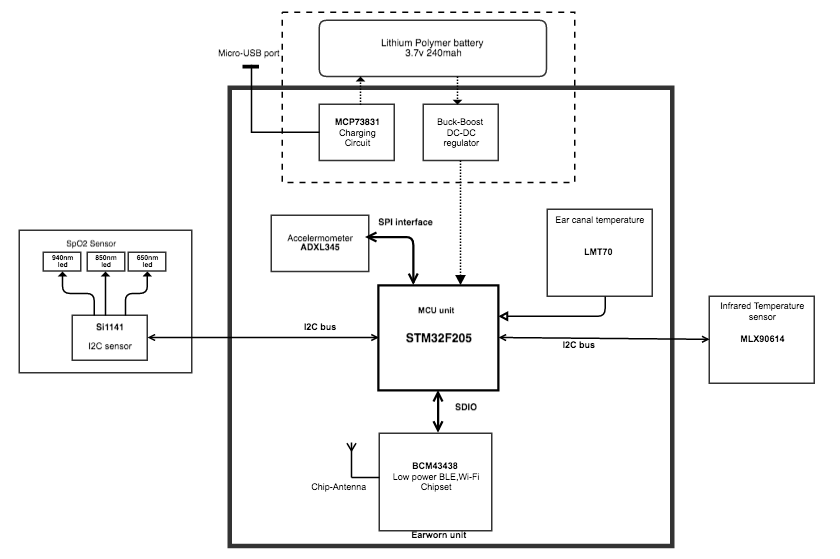
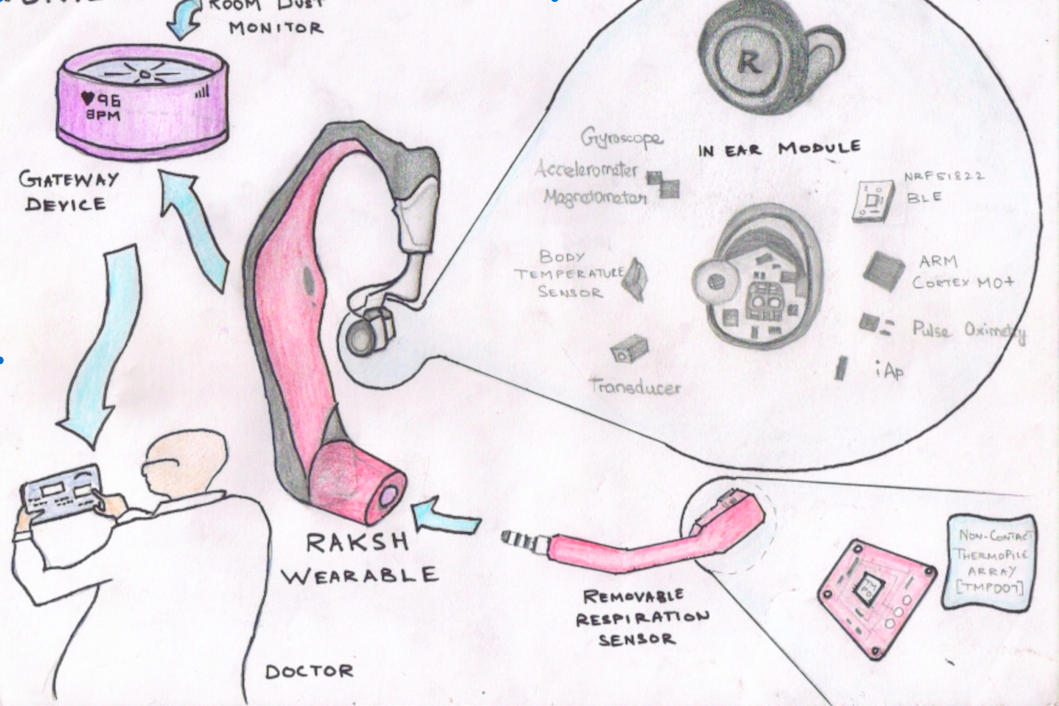
We propose a novel, inexpensive ear-worn device which would noninvasively and nonobtrusively monitor vital parameters like Respiration Rate, SpO2 levels, Heart Rate, Body temperature of a child to enable rapid diagnosis wirelessly.
System Design:
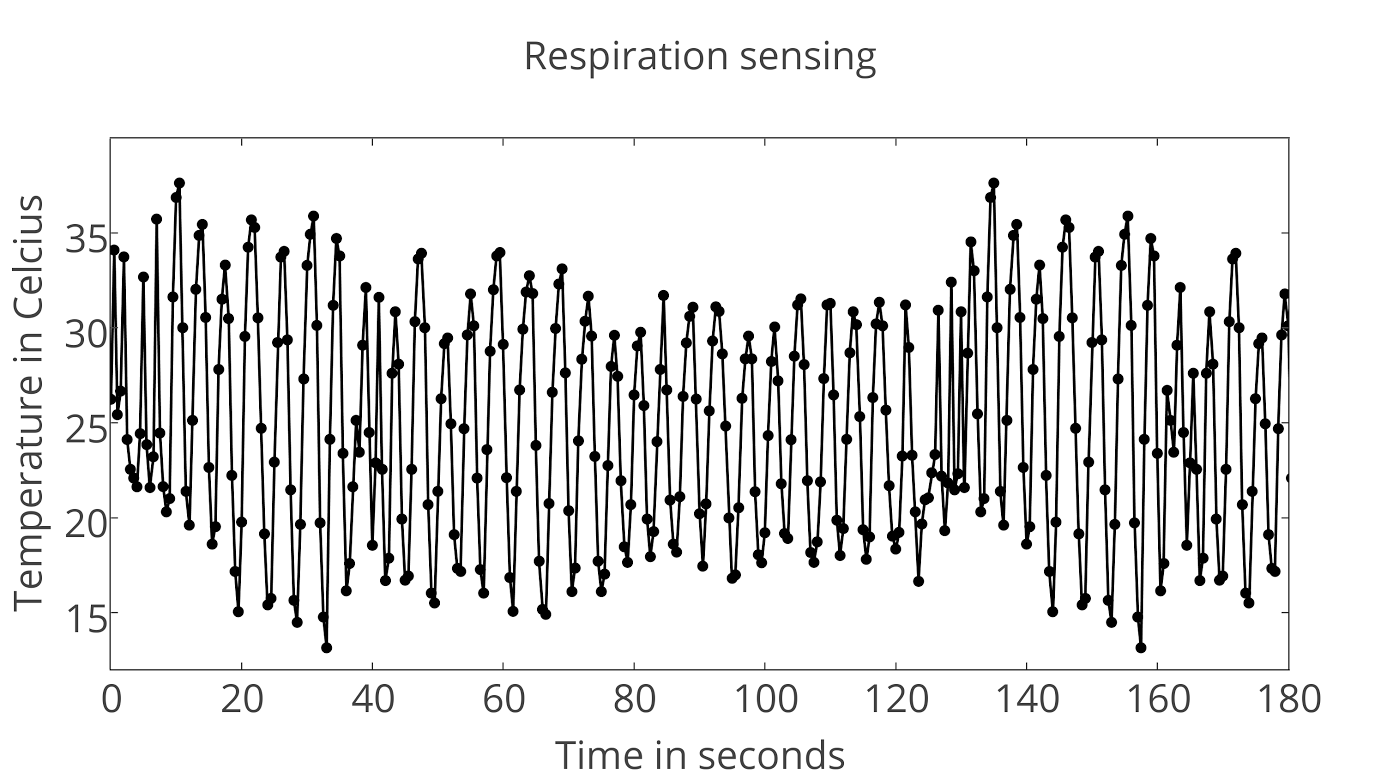
Respiration Rate Sensing:
One of the most frequently used methods to sense breathing pattern is to detect airflow using a nasal thermistor or a thermocouple sensor. We have chosen to use an IR noncontact thermopile array to measure the variation of the nasal temperature accurately using the MLX90614 noncontact infrared temperature sensor(TMP007 would be used in final design) which is pointed to the nasal passage. The sensor is smaller in size and comfortable when compared to nasal thermistors. As the child exhales, the nasal temperature increases which are picked up by the Infrared (IR) temperature sensor. The data is read at high speeds by the Microcontroller over the I2C bus. The sensor also detects ambient temperature which is used for calibration to identify threshold. The samples are compared with each other and the peaks are found. The internal timer is triggered to find the peak to peak time duration from which the respiration rate can be accurately found.
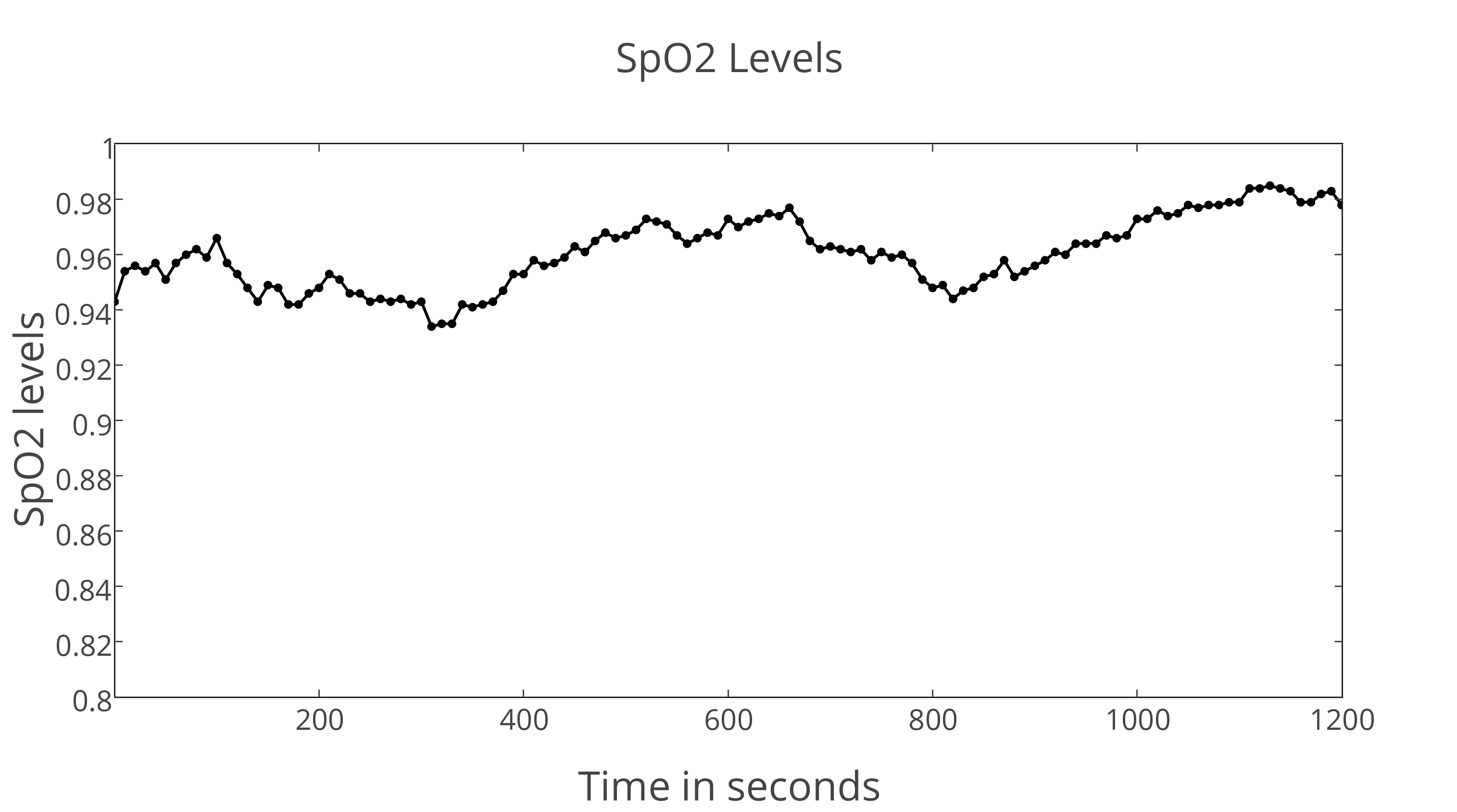
Heart Rate and Blood Oxygenation sensor:
Photoplethysmography (PPG) and Pulse Oximetry (SpO2) are carried out by a single sensor which is used to measure reflectance of three LEDs of different wavelengths. SpO2 is found by measuring the reflectance of 650 nm light in comparison with 940 nm light. Heart rate is measured by PPG wherein the change in blood volume is found by measuring reflectance of 850 nm light. The measurement of vital...
Read more » Vignesh Ravichandran
Vignesh Ravichandran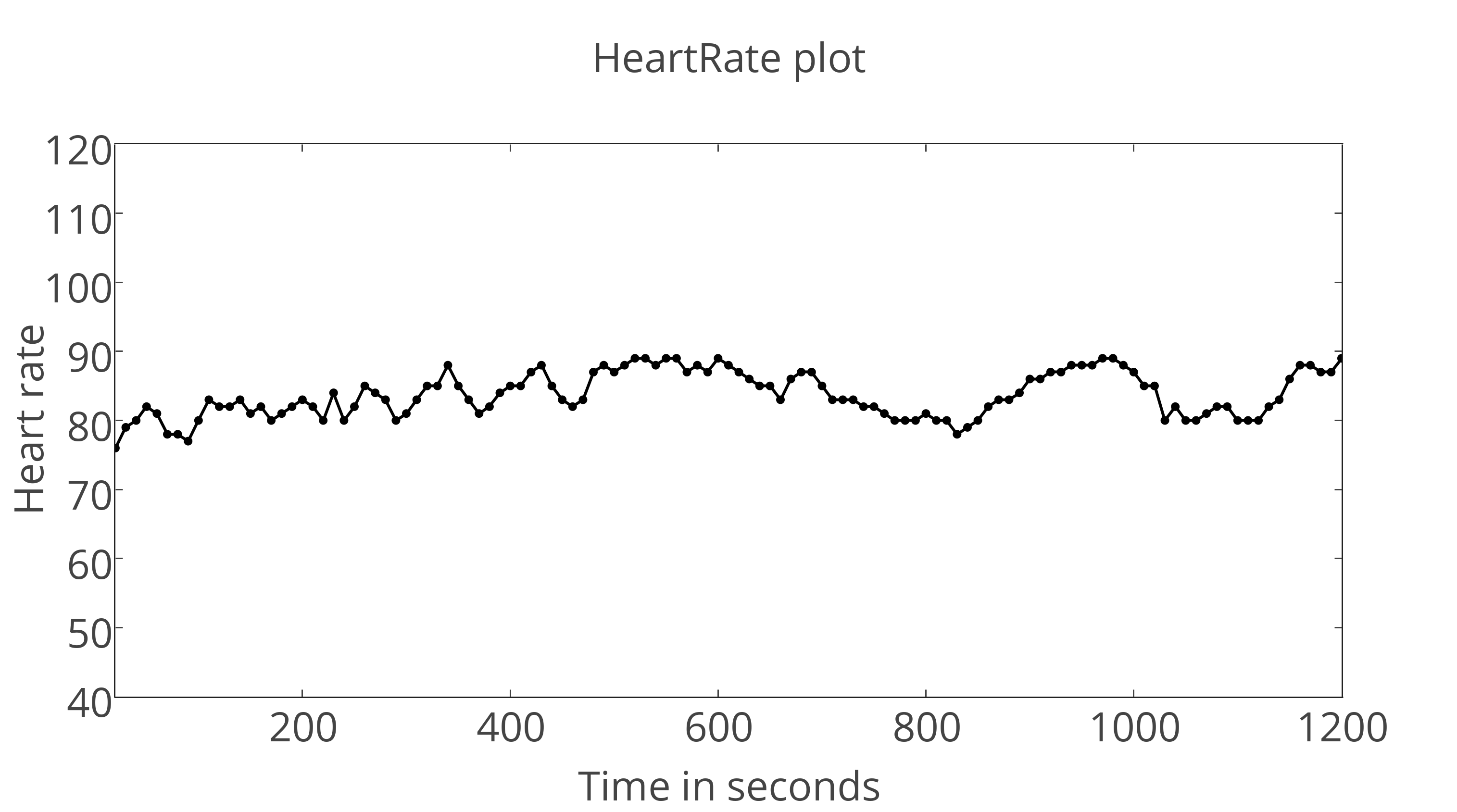






 Danie Conradie
Danie Conradie

 Vishnu Mohanan
Vishnu Mohanan
 Manoj kumar
Manoj kumar
Hi
Interesting project, have you done any work on HRV and early onset of aifb?