BACKGROUND
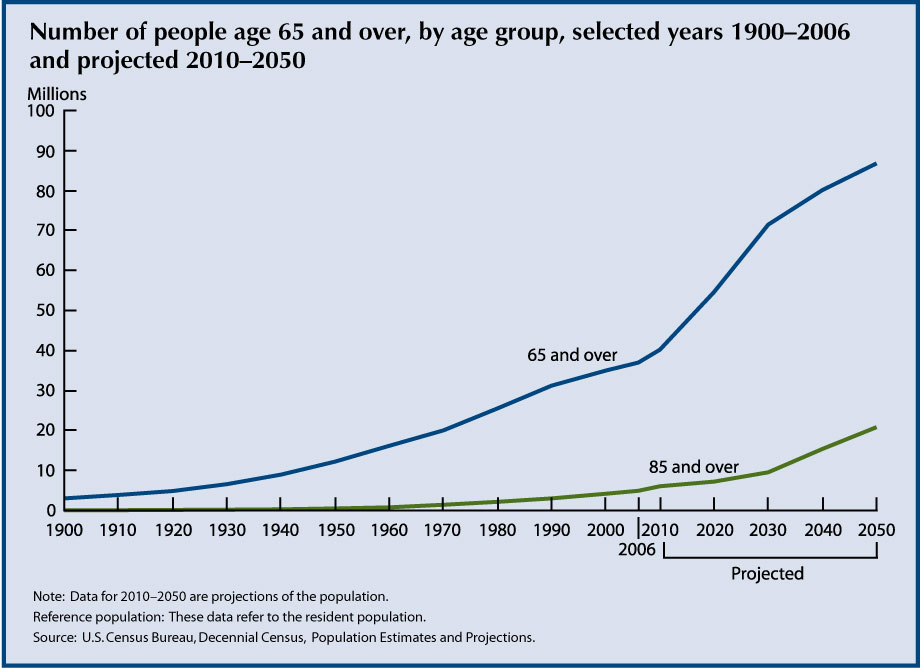
By 2030, a quarter of the population will be over the age of 65. Though life expectancy has increased significantly over the last century, complications from chronic diseases such as diabetes, heart disease, osteoporosis, and cancer often cause catastrophic events in the elderly - leading to functional decline, loss of independence, and even death.
Our team had the opportunity to shadow and work with the geriatric population the last two months in the Miami Veteran Affairs Hospital as well in the Miami Jewish Health System, a private healthcare facility for the elderly. We learned that the holistic treatment of the geriatric population addresses four domains: medical, psychological, socioeconomic, and functional. The last domain, functional, describes the ability of an individual to live independently.
To assess independence, doctors evaluate a patient's ability to perform Activities of Daily Living (ADLs) and Instrumental Activities of Daily Livings (IADLs). These tasks - eating, dressing ourselves, bathing, making phone calls - we perform every day without a second thought. However, to patients recovering from catastrophic events, these tasks may seem insurmountable.
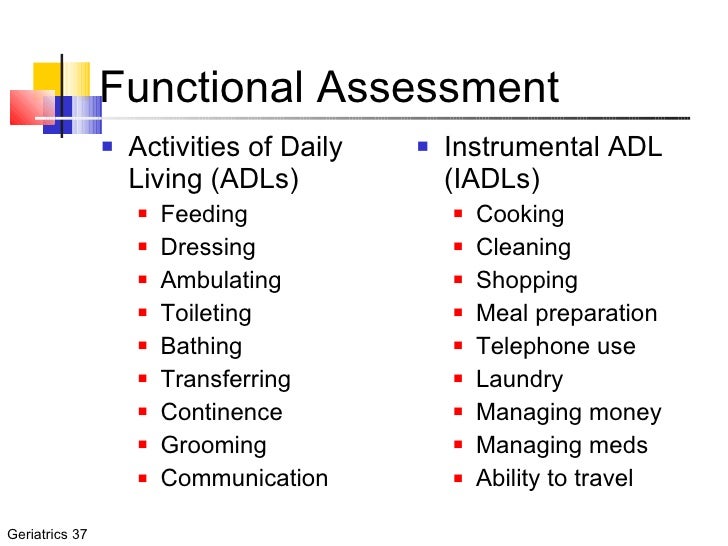
Patients who cannot perform any of the ADLs or IADLs cannot live independently in the community and depend on nurses, aides, and social workers. These individuals often have to move from their homes to assisted living and long term care facilities, at times against their will (for their safety).
After identifying and screening many potential healthcare needs of this population, we discovered that inability to transfer independently was one of the largest contributing factor to loss of independence among the elderly. Recovering from a heart attack or a bout of pneumonia, these patients are often decompensated and at a very high risk of fall. Consequently, they remain bedbound, leading to further decompensation and further loss of functionality. These patients have higher rates of mortality due to increased risk of pressure sores and infections. After witnessing this happen to many of our patients, we decided to take action.
IDENTIFYING THE PROBLEM
Rehabilitation medicine plays an essential role in helping individuals recover from acute illnesses. Physical therapists and physical medicine doctors work tirelessly to help patients become more functional and more mobile. One of the most important milestones a patient learns is the ability to transfer from the bed to the wheelchair. This is a key milestone in recovery for bed-bound patients. The ability to travel in a wheelchair exponentially increases a patient's functionality. They can now eat in the kitchen, bathe in the restroom, and better interact with their loved ones.

Use of a Hoyer Lift (image courtesy of Free Foundation)
Patients unable to transfer into a wheelchair require expensive hoyer lifts (essentially cranes operated by an assistant) or use a transfer board (essentially a wooden board that an assistant slides the patient on). It is important to note that some patients can use these independently, however this requires immense arm and wrist strength that many do not have.

Use of Transfer Board (Image courtesy of Fairview Health Services)
We decided to create a better assistive device that patients can use to reliably transfer from bed to wheelchair and back. Our device is geared toward patients with limited upper and lower extremity strength.
OUR SOLUTION
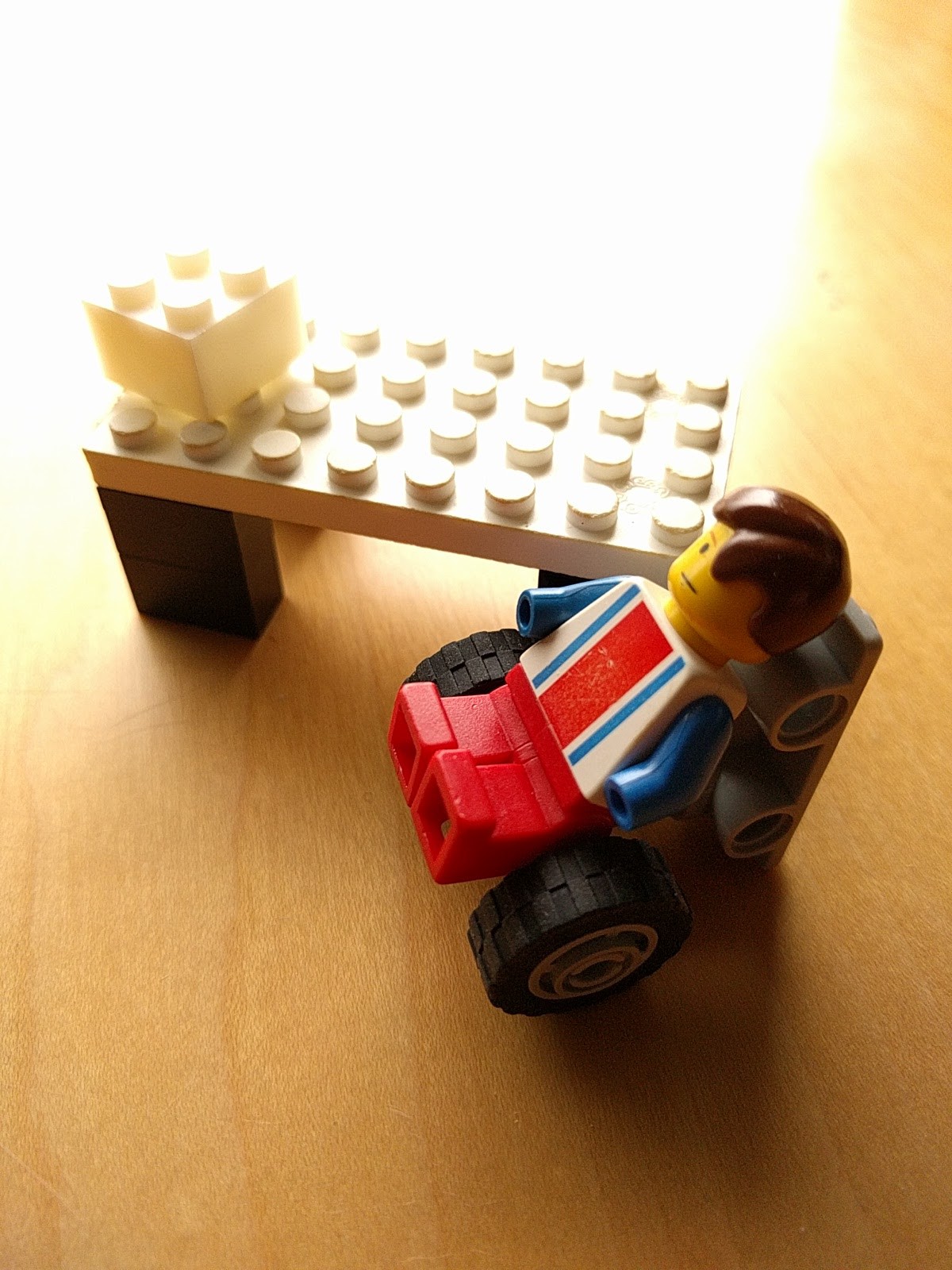
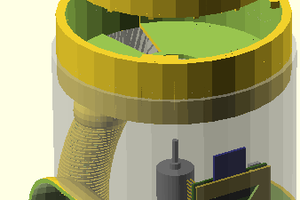
To create our device, we observed our patients, interviewed physical therapists, and actually performed hundreds of transfers on our own using the existing transfer board and various prototypes. We discovered the simplest movement for a chair bed transfer was not a lateral slide (such as the one the transfer board uses) but rather a pivot of the body. This movement is captured with our first prototype which we created with a pair of crutches.
 Louie Cai
Louie Cai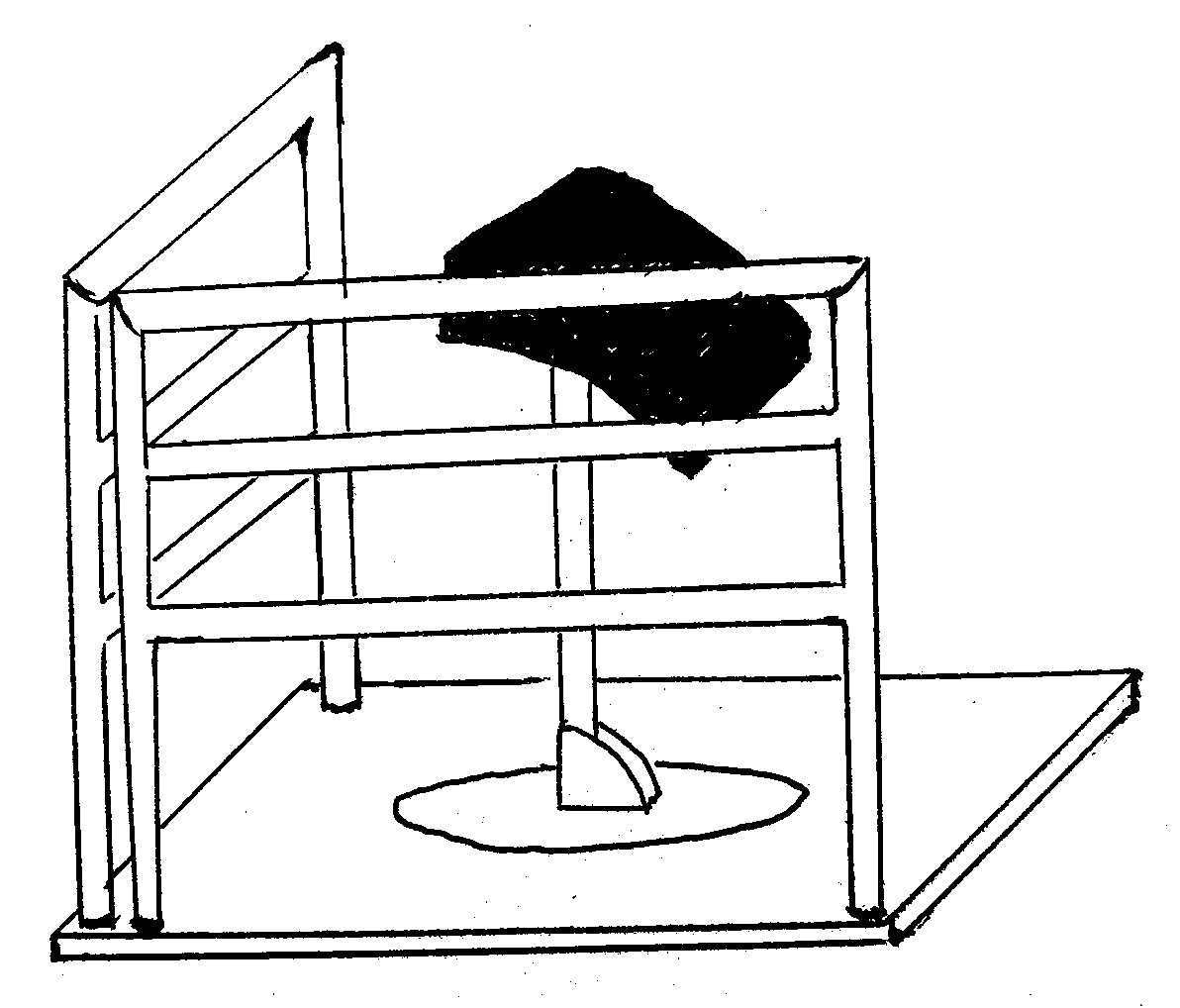




 Muhammed Azhar
Muhammed Azhar
 Ben Simms
Ben Simms
 bsutton
bsutton